Structure of the NHS
The National Health Service (NHS) is a publicly-funded healthcare system in the UK. Established in 1948, it was created to provide healthcare services to millions of people across the country. It is considered one of the largest and most complex healthcare systems in the world. The NHS provides healthcare to all of UK’s citizens, regardless of their income or social status. It is funded by taxpayers, and it provides services free at the point of use. (See: NHS Constitution: Principles and Values)
The NHS is made up of several different organisations, including hospitals, clinics, and community health services. The structure of the NHS is designed to ensure that patients receive high-quality care that is both accessible and affordable. The system is divided into three main components: primary care, secondary care, and tertiary care.
Primary Care
Primary care is the first point of contact for patients seeking medical attention. It includes services that are provided by general practitioners (GPs), community pharmacies, optometry and dental services. If there is an issue which cannot be resolved at this level, they will refer you to secondary care.
Primary care is responsible for managing the health of the population it serves. It is the backbone of the NHS, provides preventive and early intervention care, and helps to keep people healthy.
Secondary Care
Secondary care includes services that are provided by hospitals and other specialist healthcare providers. This includes surgery, diagnostic tests, and specialist consultations and treatments.
Secondary care is responsible for the treatment of more complex medical conditions that require specialised care. It is also responsible for the management of patients with long-term conditions, such as diabetes and heart disease.
Tertiary Care
Tertiary care includes highly specialised services that are provided by regional and national Centres of Excellence. This includes services such as liver transplants, cancer treatment, and highly specialised surgeries. As these centres are so specialised, they usually provide care to no more than 500 patients per year.
Tertiary care is responsible for the treatment of the most complex and rare medical conditions. It is also responsible for the training of healthcare professionals in specialised fields.
NHS Governance
Definitions
Commissioning body: The group of decision-makers who assess needs, plan, prioritise, purchase and monitor health services.
Provider: The facility that provides the health or social care.
Postcode Lottery: A term to describe how the quality of healthcare you receive depends on where you live. This is due to different spending and facilities in different regions of the UK.
Structure of Commissioning
The NHS is also governed by a number of different organisations, including NHS England, NHS Scotland, NHS Wales, and Health and Social Care in Northern Ireland. These organisations work together to ensure that the NHS is delivering high-quality care to patients across the UK.
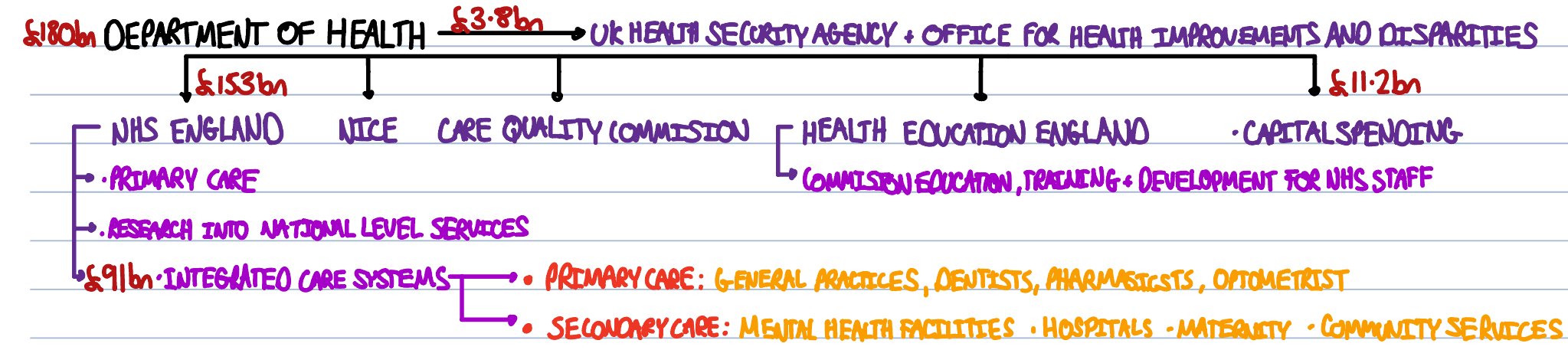
Commissioning of Financial Year 2022/2023:
This diagram shows all the commissioning bodies involved in the NHS in England to provide primary, secondary and tertiary healthcare as well as social care. A commissioning body allocates funds to a provider which provides a specific service of healthcare.
Department of Health and Social Care
The Sectary of State of Health and Social Care (in 2023) is Steve Barclay who allocates fundings to all the other commissioning bodies. In 2022/23 the department had a budget of £180bn, and it allocated the majority of its funds to NHS England. It also funds NICE, Care Quality Commission, Health Education England, UK Health Security Agency + Office for Health Improvements and Disparities and Capital Spending (investments into building and equipment). These organisations are described in more detail below.
UK Health Security Agency (UKHSA) + Office for Health Improvements and Disparities (OHID)
On the 1st of October 2021, Public Health England (PHE) officially became UK Health Security Agency (UKHSA). The majority of the roles of PHE were divided between OHID and UKHSA. The remaining duties are now commissioned directly by the Department of Health and Social Care.
UKHSA:
Responsible for protecting the population against biological (e.g infectious diseases), chemical, nuclear, and environmental threats.
Funds research, collects data, and advises governmental agencies.
OHID:
Identifies and addresses health disparities. Works to reduce inequalities in health between different communities and groups.
Takes action to improve public health including action against tobacco, obesity, and drugs.
Works with local authorities and the government to provide early diagnostic services.
Drives innovation in improving health including technology, analytics, and policies.
NHS England
NHS England is a large commissioning body who plan, prioritise and fund different groups including:
Integrated Care Boards (ICBs)- These are commissioning bodies - a component of an Integrated Care System (ICS). NHS England funds these boards relative to the size of the population in that area, the average age of population and its level of deprivation. These boards can then commission specific facilities and services.
Reserve funds for ICBs.
National Level Services - NHS England commissions some national services like rare cancer treatments.
Primary Care - In Integrated Care Systems (see below) which have not taken full responsibility for primary medical care in that area, NHS England funds some services directly. This includes primary care, offender health, military health, and veteran health.
Specialised Services - some specialised services are also commissioned directly by NHS England.
National Institute for Health and Care Excellence (NICE)
This is an institution which publishes guidance for the NHS. They:
Evaluate the most up to date research behind treatments.
Test and analyse potentially new treatments.
Produce guidance on avoiding ill-health and promoting good health.
Assess treatments on a financial and clinical basis.
Produce guidelines for investment by Integrated Care Systems/hospitals into specific treatments.
NICE was constructed to end the “postcode lottery” of healthcare (a term used to describe how the availability of treatments depended on where you live). Since 2005, the NHS in England and Wales are legally obligated to provide funding for treatments and medicines recommend by NICE’s Technology Appraisal Board.
Care Quality Commission
This is an independent regulator of health and social care in England (similar to Ofsted for schools) and produces reports on the quality of care of: care homes, hospitals, dental services, clinics, services at home, general practices, mental health facilities and community based services. These reports are then published online. The inspection team includes doctors, nurses, patients and others to evaluate the service from multiple perspectives. For inadequate establishments, it can issue warnings, restrict and even prosecute them.
Health Education England
This is a institution which works to plan, commission, recruit and develop healthcare staff. They produce guidelines and initiatives across several departments and healthcare settings in order to meet the “quality of care”, “compassion” and “working together for the patients” in accordance with the NHS Constitutional values.
Integrated Care Systems (ICS)
Following the 2022 Health and Care Act, ICSs became legal entities. There are 42 ICSs which cover the whole of England, and each ICSs covers a geographical region. Each has a population between five hundred thousand and three million. You may have come across the terms Clinical Commissioning Groups (CCGs) or Sustainability + Transformation Partnerships (STPs). However, since 2022, these have evolved into ICSs which contain both the commissioning body and the providers in a much closer interconnected partnership (whereas CCGs in the past were just the commissioning body). An ICS consists of two parts:
Integrated Care Boards (ICBs): This is the commissioning body in an ICS. This group plans, prioritises and funds the providers.
Integrated Care Partnerships (ICPs): These are the providers including local government, volunteers, community services and NHS organisations.
This new integrated system enables faster communication between providers and better communication between the commissioners and providers, compared to CCGs. This is particularly beneficial in the world of modern medicine where the majority of patients have co-morbidities, and may require many treatments from separate departments, services and community care.
The key aims of Integrated Care Systems are:
Improving population health outcomes.
Ensuring sustainable use of money and increasing the value for money.
Tackling key healthcare inequalities.